
Despite decreases in cancer death rates nationwide, a new report shows they are higher in rural America than in urban areas of the United States.
The report released Thursday by the Centers for Disease Control and Prevention found that rural areas had higher rates of new cases as well as of deaths from cancers related to tobacco use, such as lung and laryngeal cancers, and those that can be prevented by screening, such as colorectal and cervical cancers.
Differences in the incidence of cancer, or the rates of new cases, could arise because of risk factors such as smoking, obesity and a lack of physical activity, the report said.
But differences in the death rates could result from disparities in access to health care and timely diagnosis and treatment, researchers concluded. A higher percentage of rural Americans are uninsured, limiting their access to preventive services covered by insurance, according to federal health data.
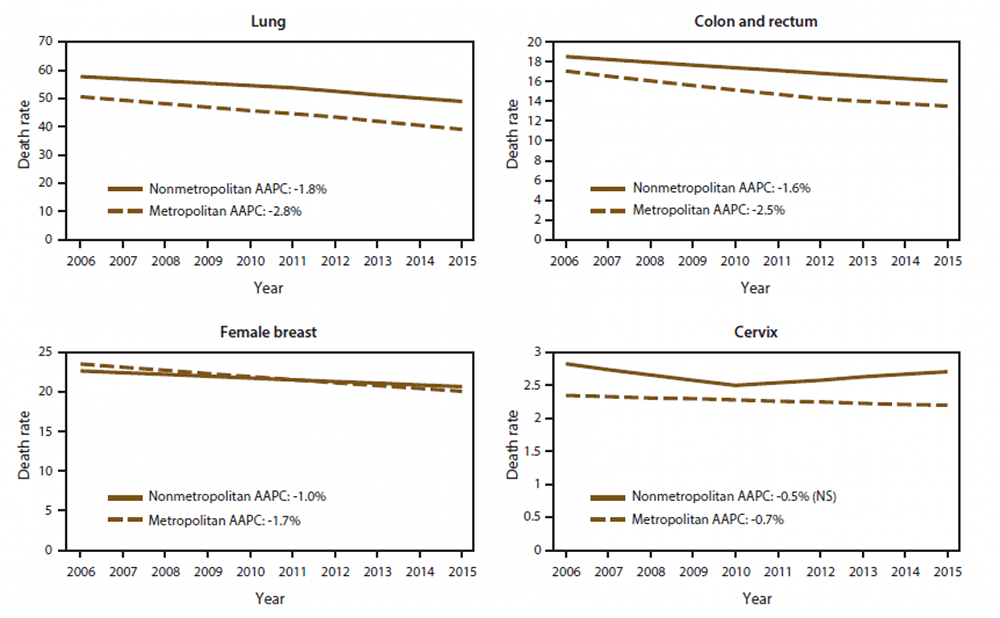
A new CDC report shows trends in annual age-adjusted death rates among people of all ages for common cancers in non-metropolitan and metropolitan counties in the United States, 2006-2015.
“While geography alone can’t predict your risk of cancer, it can impact prevention, diagnosis and treatment opportunities — and that’s a significant public health problem in the U.S.,” said Anne Schuchat, CDC’s acting director. “Many cancer cases and deaths are preventable, and with targeted public health efforts and interventions, we can close the growing gap between rural and urban Americans.”
The latest report is CDC’s first complete description of cancer incidence and mortality in rural and urban America. It adds to the troubling picture of poor health in rural parts of the country, where people are older, poorer and sicker.
More than 46 million Americans, or 15 percent of the country’s population, live in rural areas. They face numerous health disparities, compared with their urban counterparts and often are most in need of health-care services, yet have the fewest options available. As a consequence, a CDC report found this year, life expectancy is declining for rural Americans; they are more likely to die from the top five causes of death, including cancer, than their urban counterparts.
Many cancers are caused by risk factors, such as smoking, obesity, physical inactivity, alcohol use and excessive sun exposure.
In the latest CDC report, researchers analyzed cancer incidence data from the CDC’s National Program of Cancer Registries and the National Cancer Institute’s Surveillance, Epidemiology, and End Results program from 2009 to 2013. Cancer deaths were calculated from CDC’s Vital Statistics System from 2006 to 2015.
Among the findings from their analysis:
• Death rates were higher in rural areas (180 deaths per 100,000 people), compared with urban areas (158 deaths per 100,000).
• Overall cancer incidence rates were slightly lower in rural areas (442 cases per 100,000 people) than in urban areas (457 cases per 100,000), although that was not the case with some specific cancers.
• Among whites, blacks and Hispanics, overall cancer incidence rates were lower in rural counties than in other areas. But among Native Americans and Alaskan natives, the highest rates were in rural counties. Overall incidence rates among Asian Americans did not differ based on geography.
CDC researchers said several proven strategies can reduce the gaps in rates of new cancer cases and deaths. In addition to quitting smoking, limiting sun exposure, eating more healthfully, increasing physical activity and having cancer screenings such as colonoscopies and Pap tests, patients should receive the recommended vaccinations against cancer-related infectious diseases, such as human papillomavirus, officials said.
Studies show the HPV vaccine could help avert tens of thousands of cancer cases during young Americans’ lives. But the HPV vaccine remains underused, even as some of those diseases surge.
