This year, over 9,000 men will be newly diagnosed with testicular cancer. This number may be higher than you would think, considering how little we hear about this disease. In fact, testicular cancer has the highest rate of diagnoses in males age 15 to 44. The intimate and sensitive aspects of this disease can often prevent men from talking openly about it, or from asking valid questions concerning its effects – specifically when it comes to sexual health. This stigma has prevented answers to these questions from becoming common knowledge, and blocked a general open dialog about this disease.
We find that the most common questions surrounding the effects of testicular cancer and its treatment have to do with erectile dysfunction, sex drive, and fertility. Considering the nature of available treatment options, this is completely understandable. Let’s take a look at the facts.
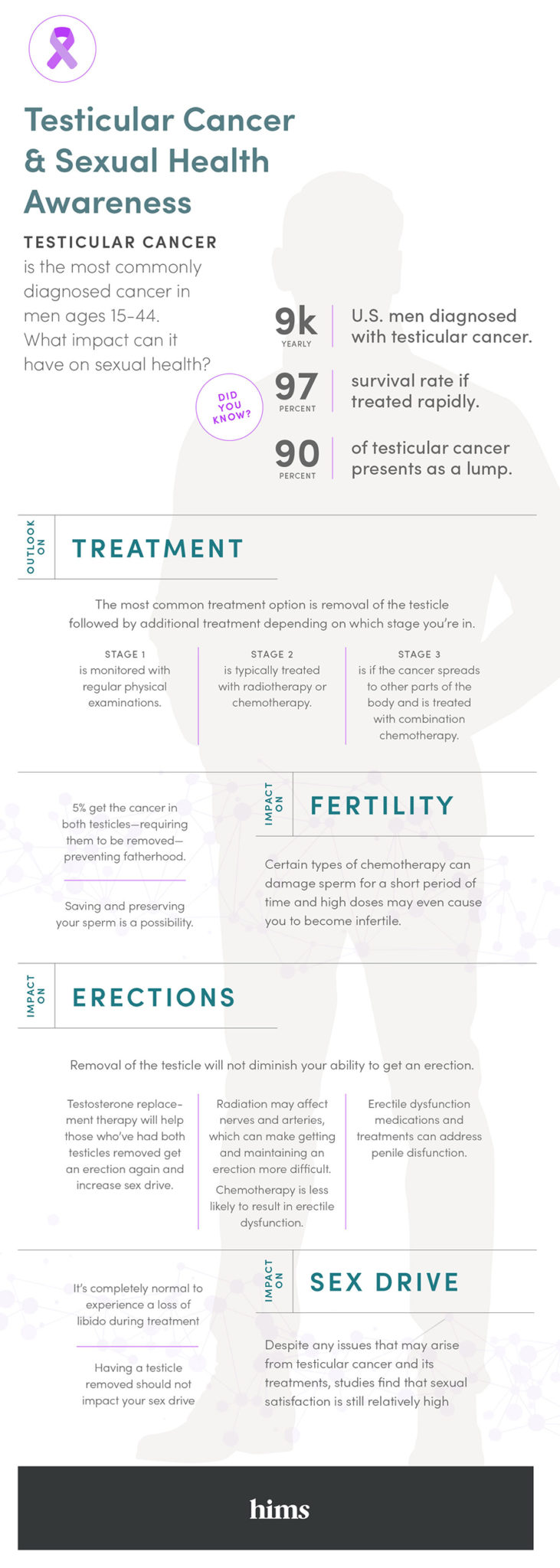
Erectile Dysfunction
Removal of the affected testicle is the most common and effective treatment for testicular cancer. While this alone will not diminish your physical ability to get an erection, patients often suffer mental and emotional effects from surgery that may cause erectile dysfunction. Losing a testicle can result in men feeling a loss of masculinity which can, in turn, lead to a lack of confidence. Certain types of radiation can also affect nerve endings and arteries in and around the scrotum, making it more challenging to get and also sustain an erection.
In these cases, patients can turn to a number of erectile dysfunction solutions. While some may feel meditation is the answer, there are also a number of men’s health brands making medicinal treatments for erectile dysfunction available online.
If both testicles have to be removed, then erectile dysfunction will be almost a certainty. In these rare cases, testosterone replacement therapy can be utilized to recapture sex drive and defeat erectile dysfunction. There are numerous forms of testosterone replacement therapy; from skin patches, to injections, and more. However, it should be known that testosterone replacement therapy does sometimes cause unwanted side effects, such as irritability, acne, and higher red blood cell counts.
Sex Drive
Experiencing a loss of libido after surgery, or in the wake of chemotherapy/radiation treatments is completely normal. Given appropriate recovery time, sex drive should return; often to pre-diagnosis levels. With the exception of having both testicles removed (which only occurs in 5% of cases), no treatment option should result in a permanent loss of sex drive. Studies even have shown that sexual satisfaction remains relatively high following effective treatment.
Fertility
Many men fear their ability to father children may be affected by testicular cancer and its treatments. Regardless of the individual diagnosis and prognosis, preserving a semen sample at a sperm bank is the best way for patients to make sure they are securing a future that includes fatherhood.
In the uncommon scenario where both testicles are removed, infertility is sadly a guarantee. But having only one testicle does not rob you of your fertility at all. Some forms of chemotherapy can temporarily damage sperm during active treatments. Over a long period of time however, this could lead to sterility. So it is important to consult with a doctor and know the potential outcomes of the prescribed chemotherapy.
Fertility is also left intact after radiation treatments. Any damage done to sperm during radiation will usually be gone after a few months. However, it is strongly suggested that men who have been treated with radiation therapy for testicular cancer, not attempt to father a child until a year after their last round of radiation therapy. This is to ensure that any and all radiation has left the body and will not be passed to the child, where it could cause health issues.
The best way to arm yourself against testicular cancer is to know the facts. See our previous post to learn more about warning signs, self-checks, and other risk factors for testicular cancer.
